ARUP Laboratories’ noninvasive prenatal testing (NIPT) uses massively parallel whole genome sequencing to provide screening for common chromosomal abnormalities. This test is powered by a fully automated workflow, thereby reducing the risk of human error and enabling decreased turnaround times.
What Is NIPT?
NIPT, also called noninvasive prenatal screening, or NIPS, is a prenatal screening test that assesses the risk that a fetus will be born with an abnormal number of chromosomes. Resulting disorders, also known as aneuploidies, include trisomy 13, trisomy 18, trisomy 21 (Down syndrome), and sex chromosome aneuploidies (SCAs).

Shelly Bosworth, MS, LCGC
Play This Video Spotlight (12 mins)
NIPT is not a diagnostic test; however, it can be used as a cost-effective, safe screening option as early as 10 weeks of gestation. A blood-based screening, NIPT will determine whether the patient is at high or low risk of aneuploidy of the fetus; the risk level will indicate whether additional confirmatory testing is recommended. If patients receive a high-risk screening result or if a result cannot be generated, additional confirmatory testing will be recommended.
Detailed information about NIPT can be found in the Prenatal Testing for Chromosomal Abnormalities and Neural Tube Defects topic on ARUP Consult.
Why Use NIPT?
NIPT is the most sensitive and specific prenatal screening option for trisomy 13, trisomy 18, and trisomy 21 (Down syndrome). It offers improved testing performance compared with traditional maternal serum screening (MSS), with fewer false-positive and false-negative results. Testing is noninvasive, requires a single tube of blood from the pregnant individual, and can be performed as early as 10 weeks of gestation and throughout the end of the pregnancy. The screening result is normally returned to the provider within 5–7 days.
- Access more detailed information about the performance of ARUP’s NIPT in the Noninvasive Prenatal Aneuploidy Screen by Cell-Free DNA Sequencing Test Fact Sheet.
- For more information on testing options, visit Prenatal Testing for Fetal Chromosomal Abnormalities and Neural Tube Defects on ARUP Consult.
Impact on Patient Care
Autosomal aneuploidies such as trisomy 13, trisomy 18, and trisomy 21 (Down syndrome) disrupt the normal course of development and cellular function in a fetus and are associated with congenital malformations, intellectual disability, and increased risk for fetal/infant mortality.
NIPT offers a noninvasive way to screen for these conditions, thereby reducing the risk of miscarriage associated with prenatal diagnostic procedures such as amniocentesis and chorionic villus sampling (CVS). NIPT results provide information to inform further testing and clinical decision-making. High-risk screening results merit prompt, appropriate follow-up, as critical clinical decisions should be based on diagnostic rather than screening test results.
NIPT can also determine fetal sex. Although parents can opt out of learning the baby’s sex, SCAs will be reported regardless of the opt-out status.
Improved Method
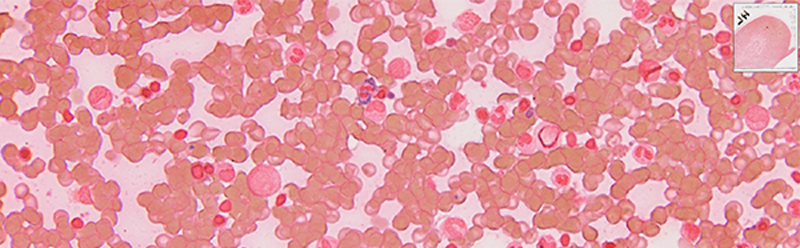
ARUP’s test is performed on the Illumina VeriSeq NIPT Solution platform, which uses massively parallel whole genome sequencing of cell-free DNA (cfDNA) derived from maternal whole blood samples. The generated paired-end sequencing data are then aligned to a reference genome and bioinformatically counted for over- or underrepresentation of the interrogated chromosomes.
Benefits of this improved method include:
- Lower sample quantity requirement
- Reduced turnaround time (5–7 days)
- Fully automated workflow, which reduces risk of human errors and improves turnaround time
To see specific metrics on test performance, including clinical and analytic sensitivity/specificity and positive predictive values, please see the Noninvasive Prenatal Aneuploidy Screen by Cell-Free DNA Sequencing Test Fact Sheet.
Why Use ARUP Laboratories?
ARUP offers the following:
- A comprehensive suite of testing for women’s health
- Clinician support from our integrated team of board-certified laboratory geneticists and genetic counselors, who specialize in prenatal genetics and can aid in test selection and result interpretation
- Results interfaced with the electronic medical record (EMR), which streamlines workflow for hospital laboratory sendout staff
- Diagnostic testing, including chromosome analysis, fluorescence in situ hybridization (FISH), or genomic microarray on amniocentesis or chorionic villus samples, available following a high-risk screen result
Professional Guidelines
The American College of Obstetricians and Gynecologists (ACOG), American College of Medical Genetics and Genomics (ACMG), and Society for Maternal-Fetal Medicine (SMFM) recommend that prenatal genetic screening, including NIPT, and prenatal diagnosis be offered to all pregnant women, regardless of maternal age or fetal risk of chromosomal abnormality.
Based on these guidelines, insurance reimbursement rates have significantly improved. Many national payers cover NIPT for women in any risk category, whereas some cover NIPT only for women considered high risk. Preauthorization may be required.
Additional Resources
ACOG Practice Bulletin: Screening for Fetal Chromosomal AbnormalitiesARUP Consult
See ARUP Consult for information on ordering recommendations, additional testing information, and test algorithms.
Prenatal Testing for Chromosomal Abnormalities and Neural Tube Defects
Educational Brochures
Education for both physicians and patients on why NIPT is important, the conditions for which NIPT screens, and important test metrics
Women’s Health: A comprehensive suite of testing for women’s health
Spotlight Video on Testing Technology: Noninvasive Prenatal Testing (NIPT) by Shelly Bosworth, MS, LCGC