Sanguine, a New Data Visualization Tool, Predicts Transfusion Needs and Provides Risk-Adjusted Benchmarking to Improve Patient Outcomes
Joshua M. Zimmerman, MD, can visualize several scenarios in which he could use granular data about a patient’s transfusion risk to better prepare his patients for surgery. With the right information, the medical director of the preoperative clinic at University of Utah Health could intervene weeks or days before a surgery to minimize a patient’s risk for transfusion.

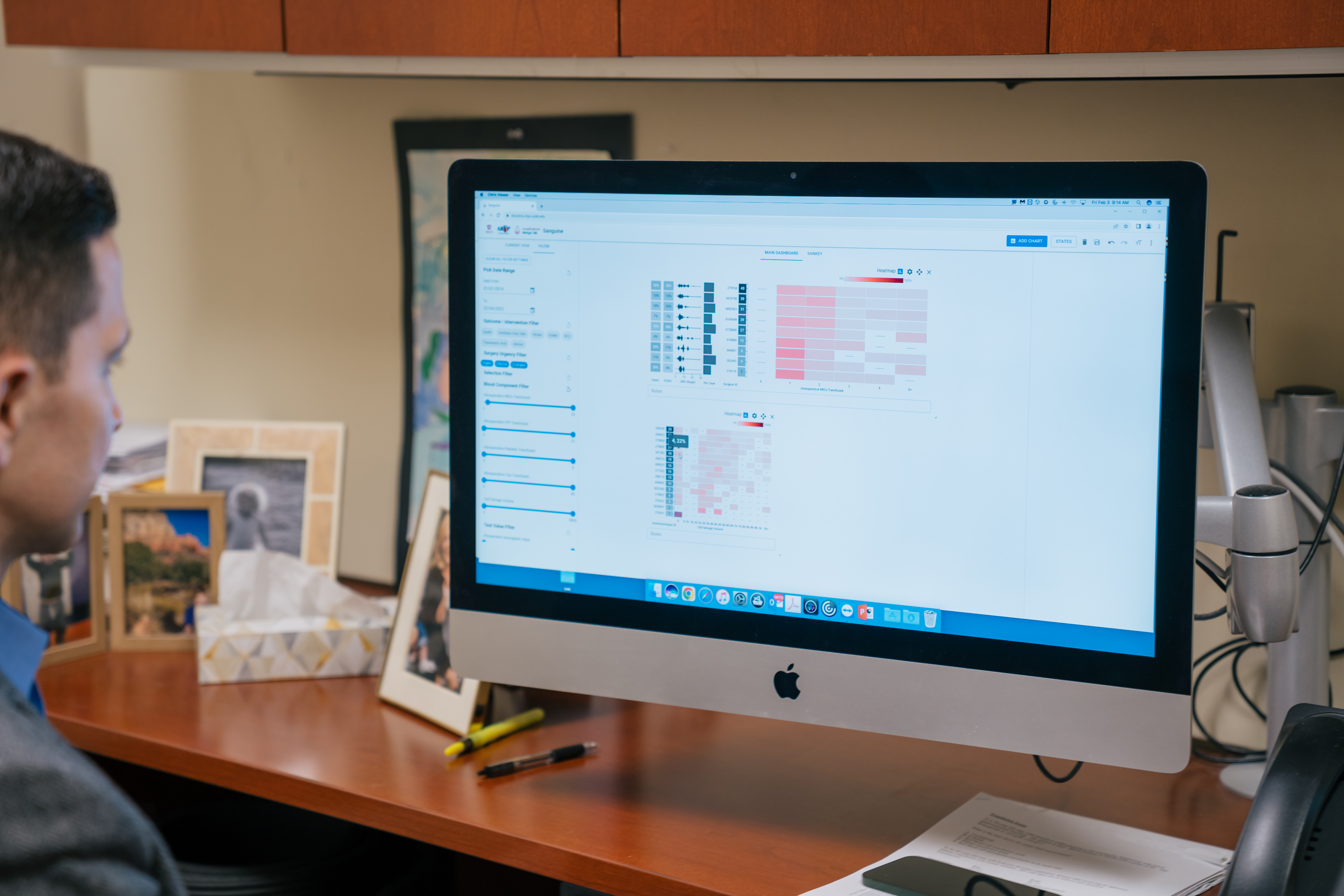
Ryan Metcalf, MD, CQA(ASQ), section chief of Transfusion Medicine at ARUP Laboratories and U of U Health and medical director of the Transfusion Service, has spent the past several years developing a tool that provides exactly the type of information Zimmerman needs. Along with a dedicated team from the University of Utah Scientific Computing and Imaging Institute (SCI)—Alexander Lex, PhD, associate professor of computer science, Haihan Lin, PhD student, and Jack Wilburn, software developer—Metcalf has developed a new data visualization tool, Sanguine, that is capable of the level of granularity and complexity required to map a truly accurate assessment of patient blood management practices.


“As valuable as it may be to have an idea of how data apply to a population, we’re never taking care of a population in the operating room. We are taking care of an individual patient,” Zimmerman said. “It’s extremely rare to have a powerful enough tool that allows us to predict the likelihood of how an individual patient will respond.”
Sanguine uses filters based on historical data to estimate how many units of blood patients might need, based on their preoperative characteristics. By using Sanguine, physicians can take measures to reduce risk by employing preoperative, preventive strategies, such as managing anemia or using cell salvage techniques, and ultimately improve patients’ surgical outcomes.

The tool also provides risk-adjusted benchmark data to help surgeons better understand how well they’ve incorporated evidence-based guidelines into their transfusion and patient blood management practices and how their patients’ outcomes compare with those of other physicians within their facility.
Metcalf hopes Sanguine will empower physicians with the insights they need to implement appropriate patient blood management strategies, an approach to transfusion medicine that optimizes transfusion practices, maximizes the use of blood products, and minimizes the need for transfusion.
“Our goal with advanced data visualization was to create a new approach to visualizing PBM [patient blood management] practices that is rapid, flexible, in context, and tied to patient outcomes,” Metcalf said. “We can build any number of customizable visualizations to rapidly access meaningful insights into the data and [gain an] understanding of practice that doesn’t really exist elsewhere, to my knowledge.”
A Patient Like Mine
Transfusion often saves lives, but it also carries significant risk of adverse effects, such as transfusion-associated circulatory overload (TACO), which occurs when blood volumes become too high and can lead to pulmonary edema. Optimizing transfusion practices and patient blood management strategies can significantly reduce risk.
“Blood transfusion is the most commonly performed procedure in the United States by far, and it’s one of the most overused procedures,” Metcalf said.
Recently, Metcalf has turned his attention to refining a feature of Sanguine he refers to as “patients like mine.” This feature allows surgeons to drill down into the data to identify past transfusion trends based on preoperative characteristics that are similar to those of their current patient.
Zimmerman, who has participated in creativity workshops during the development of Sanguine to provide his insight on preoperative challenges, often encounters preoperative anemia. To better understand where a patient’s hemoglobin levels should be before surgery, Zimmerman needs a better idea of how much blood that patient will lose during surgery.
“As simple as that question is, I don’t have a good way to understand it. I have a generic answer at a national level, but I don’t have the ability to predict that in a real patient with their surgeon and preoperative characteristics,” Zimmerman said.
With Sanguine, Zimmerman can estimate the amount of blood loss a patient will experience during surgery based on that patient’s procedure type, surgeon, and factors such as the number of red blood cell units that were transfused in similar cases. Zimmerman could evaluate a patient for iron deficiency, then decide to treat with intravenous iron to increase hemoglobin levels before surgery.
“The really valuable pieces of this are the ability to predict, not in general, not all patients on average, but how much will this patient likely need because of their preoperative and surgical characteristics,” Zimmerman said.
Zimmerman also envisions using Sanguine to better inform patients of the risks they might face during surgery.
“If a patient is likely to need 10 units of packed red blood cells during their surgery, they deserve to know that. There’s a risk that we see this as routine because it’s something we do every day, but it’s never routine to the patient. The more informed our conversations, the more informed their consent will be,” Zimmerman said.
Risk-Adjusted Benchmarking
Metcalf and his colleagues have also built a mathematical model for risk adjustment using billing code weights. This model makes it possible to examine clinical performance within various groups or hierarchies in a facility and tie that performance to important metrics for patient outcomes.
One of the biggest challenges Metcalf and his team faced is ensuring that the performance comparisons remain fair. Senior physicians, for example, may typically see patients who have more complicated or riskier conditions. Metcalf and his team performed a study to determine how best to adjust their comparisons based on risk and then incorporated it into their design.

“It’s important to treat these results as nuanced because it’s never a simple story. These are real people, and they have very complex conditions. We designed this tool very consciously to account for the many factors that play a role in risk and outcomes,” Lex said. Lex directs the Visualization Design Lab at the U and has spent his career transforming raw data into a visual, functional tool for end users.
In the next phase of the project, Metcalf and Lex want to focus on simplified visuals and a customized report that would examine cases for a particular surgeon.
“Not every surgeon cares deeply about the data, but what they do care about is their outcomes,” Lex said.
Sanguine was initially developed using data from cardiothoracic surgeries, but Metcalf plans to expand its usage to additional procedure types, particularly those that present a high risk for blood loss, such as complex cardiac surgery, liver transplant, trauma surgery, high-risk obstetric procedures, and orthopedic surgery. He plans to implement Sanguine more widely across the U Hospital later this year.
In addition to refining the usability of the tool, Metcalf is collaborating with other institutions to determine how to apply Sanguine within their facilities.
“In my view, the value of Sanguine extends far beyond transfusion medicine. This tool is tied to key patient outcomes, and it can be an example for data-driven practices for any area of healthcare,” Metcalf said.