
Interstitial lung disease (ILD) describes a large group of conditions that cause inflammation and scar tissue in the lungs.
The scarring leads to stiffness in the lungs, making it difficult to breathe.1 ILD can affect other parts of the lungs too, such as the airways, lung lining, and blood vessels. Once lung damage occurs, it is generally irreversible.
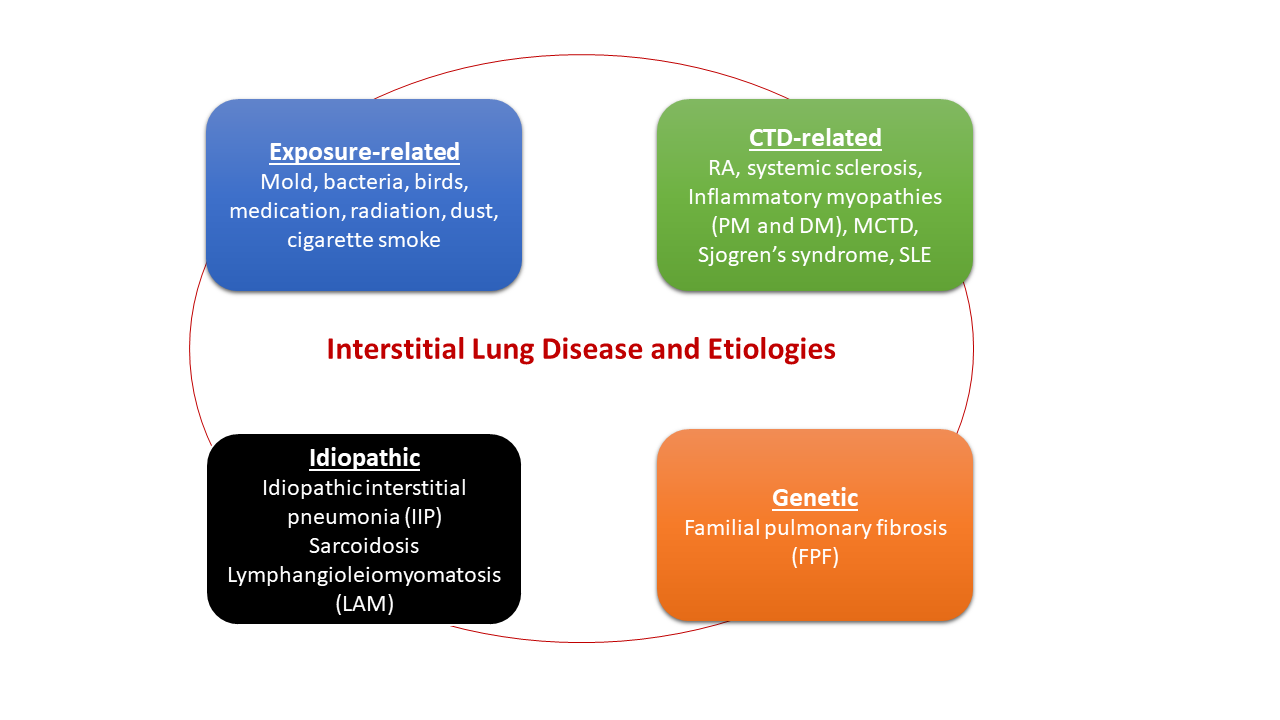
Categorization of Interstitial Lung Disease and Etiologies
ILD refers to a broad range of conditions that are generally grouped together because of common clinical, radiographic, physiologic, or pathologic manifestations. However, because their etiologies vary, they are ultimately put into one of four major categories: exposure related, genetic, connective tissue associated, or idiopathic.
Disease Presentation
ILD may be characterized by four main manifestations2:
- Respiratory symptoms (e.g., shortness of breath and cough)
- Specific chest radiographic abnormalities
- Decreased lung volume on pulmonary function test
- Characteristic microscopic patterns of inflammation and fibrosis
Disease Incidence
One study reported that 80.9 per 100,000 men and 67.2 per 100,000 women suffer from ILD in the United States, with 31.5 new cases diagnosed per 100,000 men per year and 26.1 new cases diagnosed per 100,000 women per year.4 In this study, the most prevalent ILD included pulmonary fibrosis, occupational-and environmental-associated disease, connective tissue disease-associated ILD, and sarcoidosis.
Biomarkers of Lung Injury and Inflammation
Recent evidence suggests that use of biomarkers for lung injury and inflammation may be useful in the evaluation and management of ILD. Type II counterproductive molecules, Krebs von den Lungen-6 (KL-6) and surfactant protein D (SP-D), have emerged as potential diagnostic and prognostic biomarkers of ILD. Serum levels of KL-6 and SP-D have been shown to correlate with clinical manifestations of the extent and activity of pulmonary fibrosis and inflammations. Both SP-D and KL-6 biomarkers may be helpful in monitoring patients with an established diagnosis of ILD because both markers increase with disease exacerbation and decrease with treatment and disease improvement.
Connective Tissue Disease-associated ILD (CTD-ILD)
Based on the current understanding of CTD-ILD, three main patterns have emerged from the dynamics of diagnosis.
The first and most common is ILD in a patient with established CTD. The second, which occurs in 10–30% of patients with myositis, is ILD as the first and/or only manifestation of CTD. The third and most challenging to diagnose is ILD with some autoimmune features, but not fulfilling criteria for a defined CTD. This last group of patients has recently been defined as interstitial pneumonia with autoimmune features (IPAF).
If CTD-ILD is suspected, recent guidelines recommend testing for anti-nuclear antibodies, rheumatoid factor, and anti-citrullinated cyclic peptide antibody with additional autoantibody evaluation for selected cases guided by patient’s clinical history and presentation. Due to the syndromic nature of CTD-ILD, it may be helpful to utilize a panel of autoimmune markers in disease evaluation. The connective tissue diseases associated with ILD:
- Rheumatoid arthritis
- Systemic sclerosis
- Interstitial lung disease (polymyositis)
- Dermatomyositis
- Mixed connective tissue disease
- Sjogren syndrome
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis is a rare form of ILD caused by repeated exposure to certain fungal, bacterial, reactive chemical particles, or animal proteins in certain individuals due to genetic risk factors. These agents in the environment trigger the host immune systems, causing inflammation, especially in a part of the lungs called the interstitium. In addition to family history and genetics, certain occupations and lifestyle habits may increase the risk for hypersensitivity pneumonitis.
Laboratory Evaluation of ILD
For additional information refer to our Laboratory Test Directory regarding Interstitial Lung Disease (ILD) Biomarkers Panel.
Additional Resources
- ARUP Consult – Interstitial Lung Disease
- ATI – Idiopathic Inflammatory Myopathies (Myositis)
References
- American Lung Association https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/interstitial-lung-disease/
- American Thoracic Society https://www.thoracic.org/patients/patient-resources/breathing-in-america/resources/chapter-10-interstitial-lung-disease.pdf
- Healthline https://www.healthline.com/health/interstitial-lung-disease
- Coultas DB, Zumwalt RE, Black WC, Sobonya RE. The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med 1994;150:967–972.
- ScienceDirect https://www.sciencedirect.com/science/article/abs/pii/S0031302518305488
















